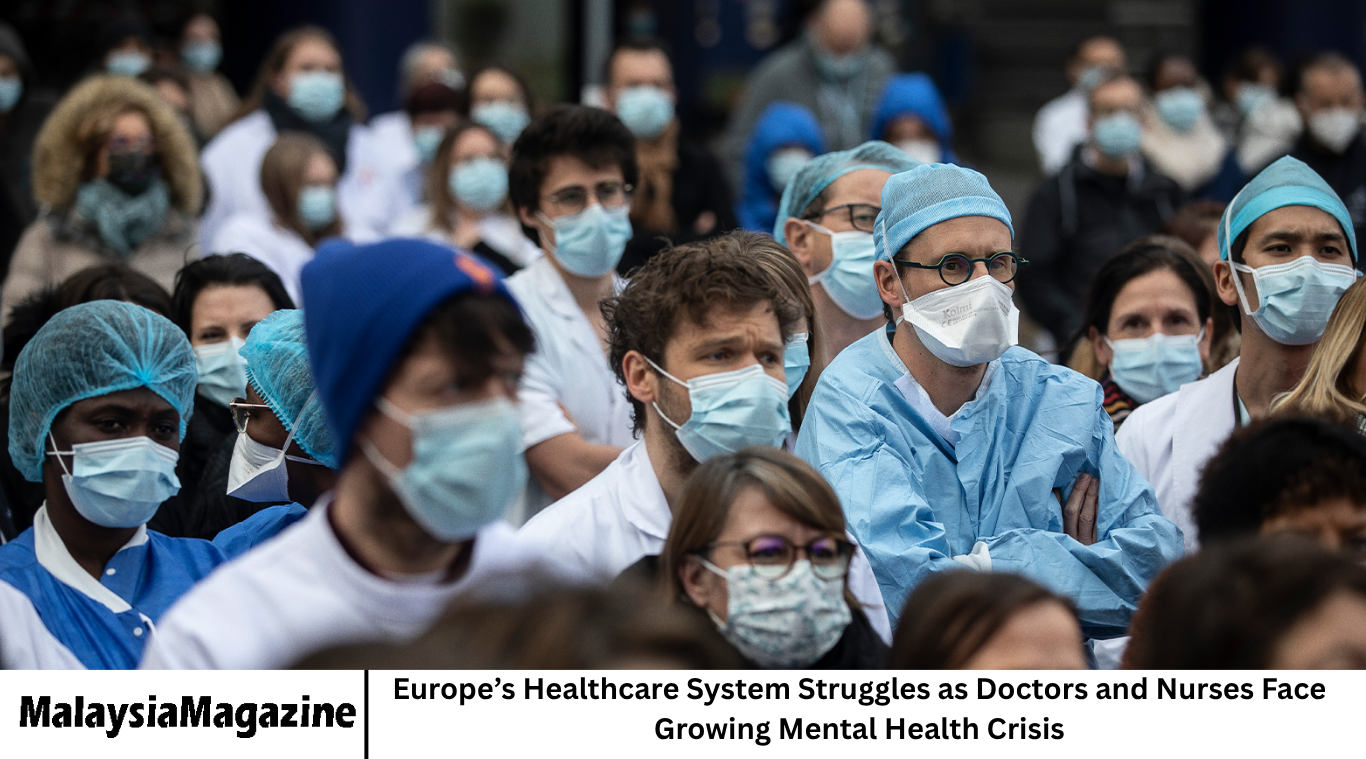
Across Europe, healthcare workers are facing a serious and growing mental health crisis. Doctors, nurses, and other frontline professionals are struggling under the immense pressure of long working hours, staff shortages, and emotional exhaustion. As hospitals continue to face heavy workloads, the mental well-being of those who keep the system running is reaching a breaking point.
- The Rising Mental Health Burden in European Healthcare
- Shortage of Healthcare Workers
- The Emotional Toll on Doctors and Nurses
- Impact on Patient Care
- National Responses Across Europe
- Burnout: The Hidden Epidemic
- The Role of Leadership and Management
- Need for Mental Health Training and Support Systems
- Technology and Innovation in Reducing Stress
- The Importance of Work-Life Balance
- Public Recognition and Social Support
- The Role of Governments and Health Institutions
- Learning from the Pandemic
- A Call for Cultural Change
- Frequently Asked Questions
- Why are doctors and nurses in Europe facing a mental health crisis?
- How does burnout affect healthcare systems?
- What are governments doing to address this problem?
- How can hospitals support their staff’s mental health?
- Why is stigma a barrier to seeking help?
- Can technology help reduce stress for healthcare workers?
- What long-term changes are needed?
- Why does this issue matter to the public?
- Conclusion
This growing challenge is not only affecting the lives of medical staff but also putting Europe’s entire healthcare system under strain. Mental health problems among healthcare professionals can lead to burnout, absenteeism, reduced patient care quality, and a shrinking workforce — all of which threaten the stability of healthcare services across the continent.
The Rising Mental Health Burden in European Healthcare
The COVID-19 pandemic exposed many weaknesses in Europe’s healthcare systems, particularly in how they handle staff mental health. Even years later, many workers have not fully recovered from the trauma of the pandemic. Hospitals are once again operating at or beyond capacity, with doctors and nurses facing intense workloads and emotional challenges.
Many healthcare professionals report symptoms of depression, anxiety, and burnout. According to recent studies from various European countries, nearly half of nurses and a significant number of doctors are experiencing mental fatigue. The constant exposure to suffering, high patient loads, and lack of support are taking a heavy toll.
Shortage of Healthcare Workers
Europe is facing one of its worst healthcare staffing shortages in decades. The World Health Organization has warned that many European nations will face severe shortfalls of doctors and nurses by the end of this decade. Retirements, migration, and burnout are making it difficult to maintain adequate staffing levels.
As the workload increases, existing staff are forced to take on extra shifts and handle more patients than ever before. This has created a cycle where mental stress leads to staff quitting, which in turn increases pressure on those who remain. Without immediate action, experts fear the situation could escalate into a full-blown healthcare crisis.
The Emotional Toll on Doctors and Nurses
Beyond physical exhaustion, healthcare workers are suffering from emotional distress caused by constant exposure to illness, death, and patient suffering. Many nurses and doctors feel that they are unable to provide the level of care their patients deserve because of time and resource constraints. This sense of helplessness adds to their stress and guilt, further worsening their mental health.
Healthcare professionals often struggle to talk about their emotions due to the culture of toughness within the medical field. The fear of being seen as weak or unfit for the job stops many from seeking help. As a result, problems like depression and anxiety often go unnoticed until they become severe.
Impact on Patient Care
When doctors and nurses are mentally and physically exhausted, the quality of patient care inevitably suffers. Fatigue and burnout can lead to mistakes, slower response times, and reduced empathy toward patients. In extreme cases, staff shortages have forced hospitals to reduce services or close wards temporarily.
Patients are also affected by longer waiting times and reduced availability of specialists. This situation highlights how mental health among healthcare professionals is not just a personal issue — it is a critical public health concern.
National Responses Across Europe
Different European countries are responding in different ways to this growing crisis. Some governments have launched mental health support programs for healthcare workers, offering counseling and stress management resources. Others are investing in workplace reforms, including better staffing policies, higher salaries, and improved working conditions.
For example, the United Kingdom has introduced well-being hubs within hospitals to help staff manage stress. France and Germany have started new initiatives focusing on work-life balance, while Nordic countries are emphasizing preventive care and employee support programs.
However, experts argue that these measures are still not enough. The mental health crisis among healthcare workers requires structural changes, not just short-term fixes.
Burnout: The Hidden Epidemic
Burnout has become one of the most common and serious issues among healthcare staff. It is a state of emotional, mental, and physical exhaustion caused by prolonged stress. Symptoms include fatigue, detachment, low motivation, and decreased performance.
In hospitals across Europe, burnout is affecting productivity and morale. Many nurses have left the profession entirely, while younger doctors are reconsidering their career choices. This loss of skilled professionals weakens the overall healthcare infrastructure and creates challenges for training new recruits.
The Role of Leadership and Management
Hospital management and healthcare leaders play a vital role in addressing mental health issues among staff. Creating a supportive and understanding work environment is essential for recovery and prevention. Leaders need to encourage open communication, provide emotional support, and promote regular mental health assessments.
Transparent scheduling, fair workloads, and flexible work options can make a major difference in reducing stress. Hospitals that focus on staff well-being often see better teamwork, lower absenteeism, and higher patient satisfaction.
Need for Mental Health Training and Support Systems
Mental health support must become a permanent part of healthcare systems, not just an emergency response. Regular mental health training can help doctors and nurses recognize early signs of burnout in themselves and their colleagues.
Support systems like confidential counseling, peer support groups, and mental health leave policies are necessary to ensure staff feel safe seeking help. Additionally, mental health education should be part of medical and nursing school curricula, preparing future professionals to cope with emotional challenges.
Technology and Innovation in Reducing Stress
Technology can play an important role in reducing workplace stress. Digital health systems, automation, and telemedicine can simplify routine tasks, reducing the workload for healthcare staff. For instance, AI-assisted tools can help doctors analyze data more efficiently, freeing up time for patient care.
However, technology should be implemented thoughtfully. Poorly designed digital systems or excessive reliance on data entry can actually increase stress. Balancing human interaction with digital efficiency is key to ensuring positive results.
The Importance of Work-Life Balance
Achieving work-life balance is essential for maintaining mental health. Many European healthcare workers work long shifts, often with limited rest periods. This imbalance not only affects mental health but also physical health and family life.
Policies that support flexible working hours, adequate rest days, and mental health breaks can make a big difference. Hospitals that have adopted such measures report lower staff turnover and improved job satisfaction.
Public Recognition and Social Support
During the pandemic, healthcare workers were celebrated as heroes. However, that public appreciation has faded for many, even as the workload remains heavy. Continued recognition and respect for their hard work are vital to maintaining morale.
Public campaigns that highlight the mental health struggles of healthcare workers can also help reduce stigma and encourage more open conversations about emotional well-being.
The Role of Governments and Health Institutions
Governments across Europe must invest more in healthcare workforce support. This includes funding for recruitment, training, mental health programs, and working condition improvements. Without such investment, the mental health crisis will continue to deepen, leading to long-term damage to healthcare systems.
Health institutions also need to adopt sustainable practices. Instead of temporary relief efforts, they must build lasting frameworks for staff welfare, such as dedicated mental health departments and employee assistance programs.
Learning from the Pandemic
The pandemic taught valuable lessons about resilience, teamwork, and the importance of mental health in healthcare. While it exposed weaknesses, it also showed that collective action can bring meaningful change. Hospitals that prioritized staff mental well-being during COVID-19 were better able to cope with pressure and maintain quality care.
Moving forward, those lessons should be used to create a culture of empathy, flexibility, and respect in healthcare workplaces.
A Call for Cultural Change
Addressing the mental health crisis among healthcare workers requires a cultural shift. The mindset that healthcare professionals must always remain strong needs to change. Compassion and vulnerability should be recognized as strengths, not weaknesses.
Encouraging openness about mental health, promoting teamwork, and ensuring emotional support can help build a more humane and sustainable healthcare system.
Frequently Asked Questions
Why are doctors and nurses in Europe facing a mental health crisis?
They are facing a crisis due to long working hours, staff shortages, emotional stress, and lack of adequate mental health support in hospitals.
How does burnout affect healthcare systems?
Burnout leads to lower productivity, higher error rates, staff shortages, and declining quality of patient care.
What are governments doing to address this problem?
Some European governments have launched wellness programs, provided mental health resources, and introduced better working conditions, but more systemic action is needed.
How can hospitals support their staff’s mental health?
Hospitals can offer counseling services, mental health leave, flexible schedules, and create supportive environments that encourage open discussion.
Why is stigma a barrier to seeking help?
Many healthcare professionals fear that seeking mental health support could be seen as a sign of weakness or may affect their careers.
Can technology help reduce stress for healthcare workers?
Yes, technology can streamline tasks, automate data management, and improve efficiency — but it must be implemented carefully to avoid adding new pressures.
What long-term changes are needed?
Structural reforms, better funding, cultural change, and continuous mental health programs are needed to ensure lasting improvement.
Why does this issue matter to the public?
Because the mental health of doctors and nurses directly affects the quality of care patients receive, making it a shared concern for all.
Conclusion
Europe’s healthcare system is facing one of its most significant challenges — the mental health crisis among doctors and nurses. These professionals are the backbone of healthcare, yet many are struggling silently with stress, burnout, and emotional exhaustion.
To protect both healthcare workers and patients, governments, institutions, and communities must work together to create systems that value mental well-being as much as physical health. Better staffing, fair pay, emotional support, and cultural change are essential steps toward building a healthier, more resilient future for Europe’s healthcare system.